Systems4PT’s Guide to Patient Billing and Collections
Systems4PT is excited to offer this exclusive new support series to all Systems4PT members. Our series “Patient Billing and Collections“ covers utilizing Systems4PT to manage patient billing effectively and efficiently. We hope this information will improve your understanding of the data’s meaning and how to use it.
Part One: Verifying Patient Benefits
Verifying Patient Benefits
Verifying your patient’s insurance benefits before their first appointment is critical in successful billing, collections, and cash flow for your clinic. Multiple sites are available for obtaining these benefits, and you should utilize whichever one you are most comfortable with and provides the most reliable information. Systems4PT provides an online Patient Eligibility Technology (PET) link directly from the V & A screen, where you will enter this information.
The following download has step-by-step instructions for utilizing the PET.
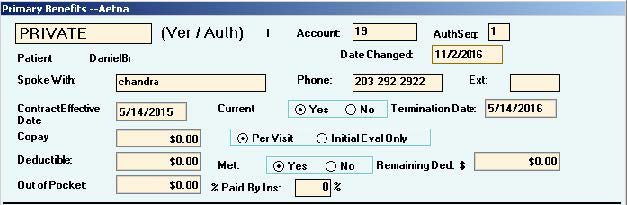
The V and A Screen
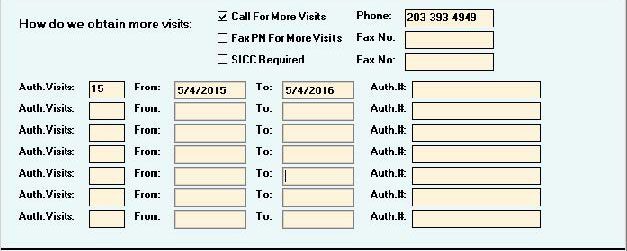
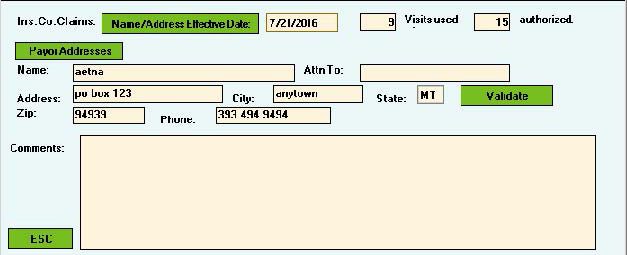
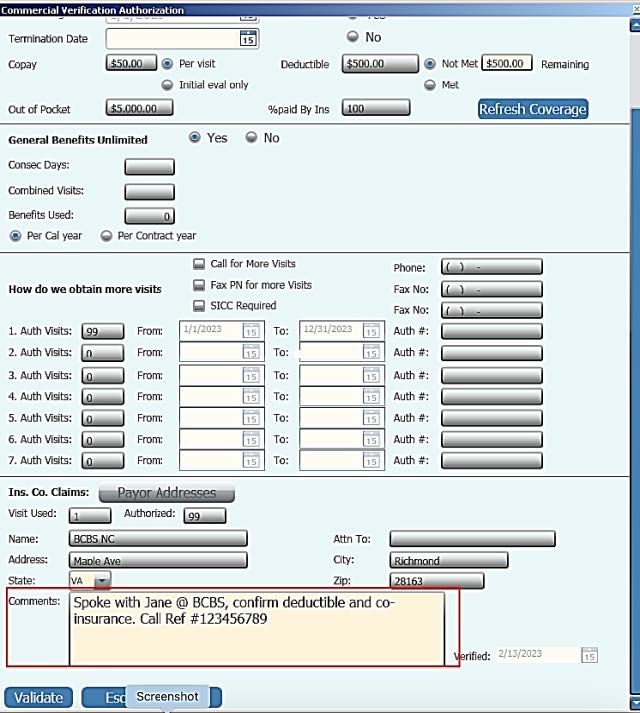
Accurately completing the V & A screen is a crucial step for successful billing, collections, and cash flow for your clinic. The first block of this screen contains critical information regarding the costs the patient will be responsible for. By correctly entering this information, it will appear on the Patient Processing Screen (PPS) each time you check in a patient, and you will be able to collect from the patient at the time of service. You do not want to have to chase down this money at a later date!
Block One
Block Two
Block Three
Block Four
Block #1
This is the crucial information for your Patient Billing & Collections and the only block discussed in this series.
- When you do not need to call the insurance, type which website you obtained the information from. E.g.: PET, ASHlink, Availity, OptumHealth, CIGNAforHCP, etc.
- After calling for benefits, enter the phone number that you called and the applicable extension.
- If you do not call for benefits, record the phone number for “Provider Services” from the patient’s insurance card.
- Obtain the start date of the patient’s insurance policy. This is frequently the first of the year but not always, so be sure to verify. If you are advised that the patient’s policy is terminated, mark “No” for current and enter the termination date.
- Next, check if the patient has a co-pay, co-insurance, or both. Enter the co-pay amount in the box and check “Per Visit” or “Initial Evaluation Only” depending on what you were advised.
- For patients with co-insurance, you will enter the amount that the insurance company pays in the box “% paid by insurance”.
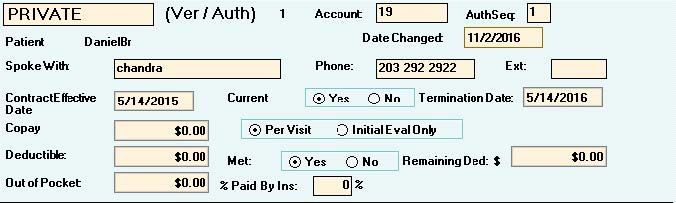
Anytime you call for benefits, always get the name of the person you spoke with. Also, request a “Call Reference Number” at the end of the call and document that number in Block #4 “Comments.” Comments entered in Block #4 do not populate anywhere else in Systems4PT.
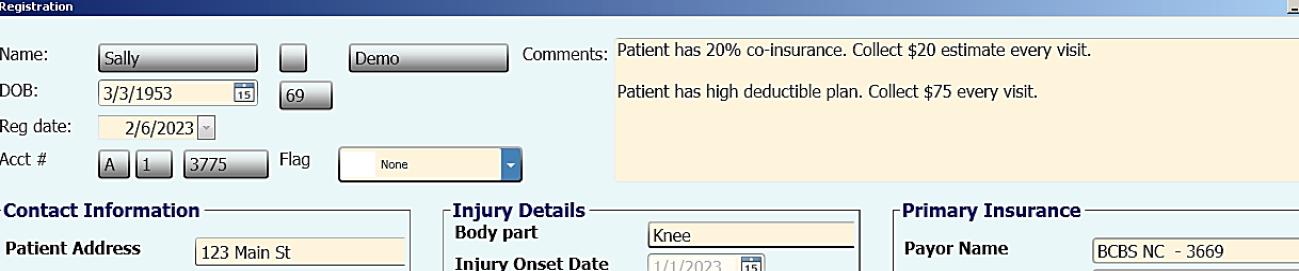
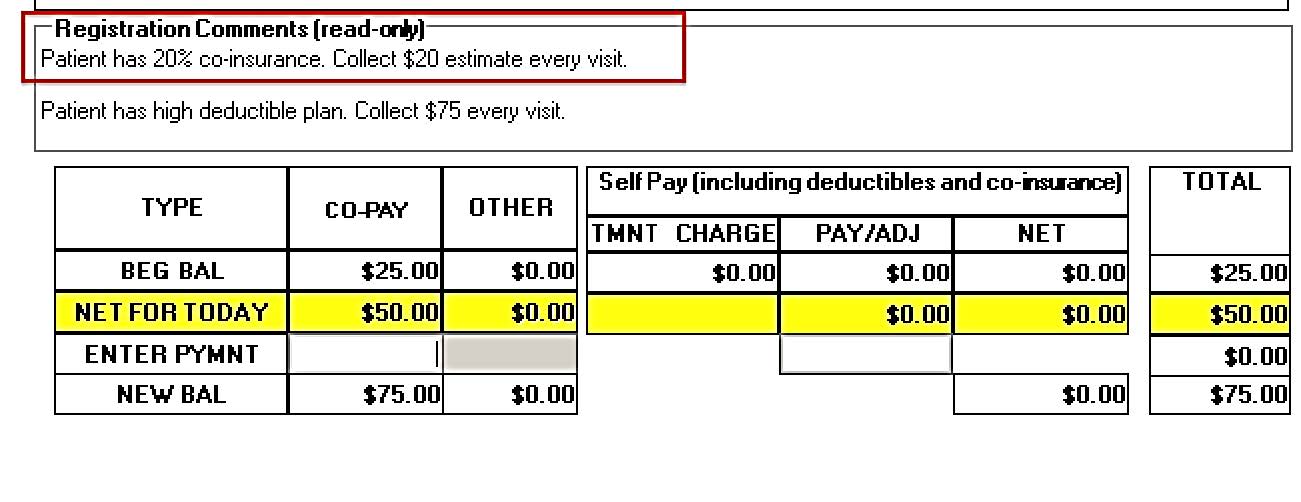
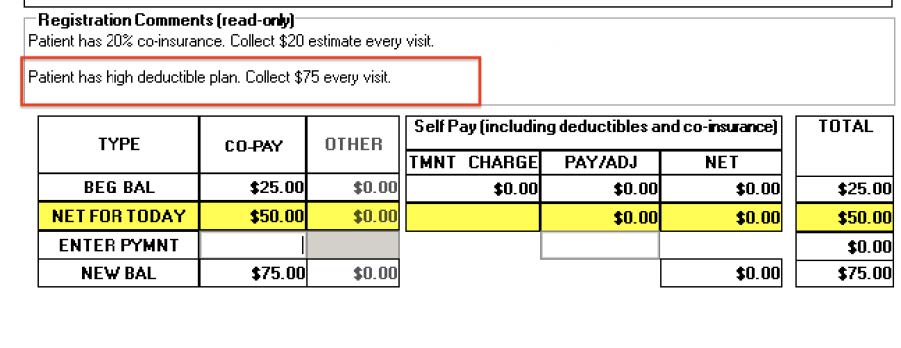
There are a couple of options for collecting this co-insurance at the time of service. If your contract is a flat rate fee, you can calculate the appropriate percentage for that fee. Enter this number in the “Comments” section of the Patient Registration screen with a note to collect each visit. This note will appear in the Patient Processing Screen (PPS) each time the patient is checked in. E.g., Flat fee rate of $100 per visit. Co-insurance of 20%. Collect $20 for every visit.
Patient Registration
Patient Processing Screen
However, if your contract is a fee schedule, collecting this amount at the time of service becomes a little more difficult. In this situation, the patient’s treatment may vary daily. Depending on the treatment rendered that day, the therapist may bill different CPT codes or different unit quantities. It is rarely efficient to try and gather the billing data for that day’s treatment, apply the fee schedule, and calculate the patient’s percentage while the patient is still in the clinic. Consequently, this usually leads to friction between the treating therapist and the front desk member. Options for this scenario will be explored more in Part III: Patient Processing Screen, of our series.
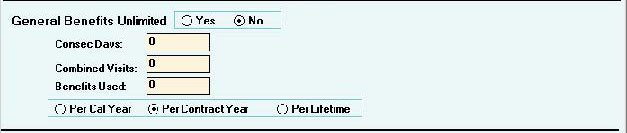
Deductible
Next, look for whether the patient has a deductible and, if so, how much has been met. Enter the deductible amount. If it has not been met, enter the amount remaining as of the date you verified the insurance benefits.
It is very important to be aware that the deductible is met in the order that the payor receives the claims, not by order of the service dates. There is a possibility that your patient has had other medical treatments, and other providers have already “collected” their deductible. Still, the deductible will be taken from your payments if your claims are received and processed before these other claims. The patient will be responsible for paying that amount to you. It is always a good idea to explain that to the patient so there are no surprises.
If the patient has a high deductible insurance plan, you want to be collecting this amount at the time of service! If your contract is a flat rate fee with the payor, collect the full amount of that rate every visit. Put a note in the “Comments” box on the registration that states, “Collect $xx every visit for deductible,” and this will appear on the PPS each time your front desk checks in the patient.
Patient Registration
Patient Processing Screen
If the insurance is a fee for service, calculate your average re-imbursement for that payor and collect this amount each visit from the patient. Advise the patient that this is an estimate, and the difference will be reconciled at the end of treatment after the insurance company has processed all the claims.
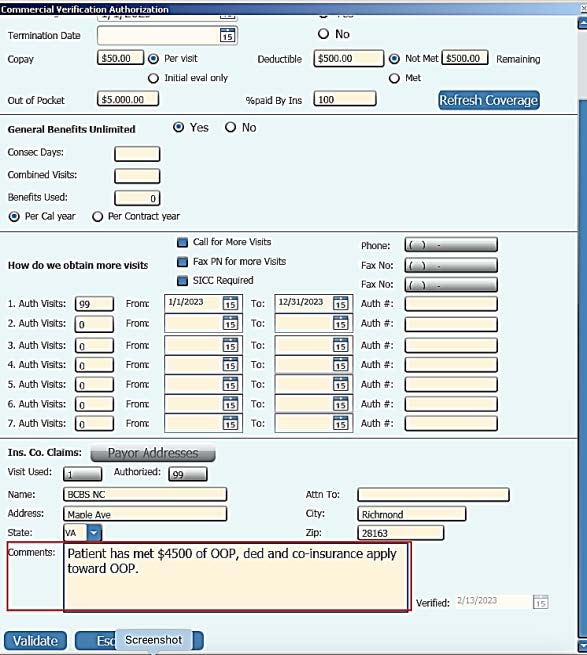
Finally, find the patient’s “Out-of-Pocket Maximum” for the year. This is the amount that the patient must pay before the payor will cover expenses at 100%. There is no box to enter how much of that amount they have met at the time you verify benefits, but it is recommended that you record that number in Block #4 “Comments”. You should attempt to determine if the patient’s co-pays count toward that out-of-pocket maximum.
If you need step-by-step instructions on completing the entire V & A Screen, click the button below.
Check out ALL the great articles in Systems4PT’s Guide to Patient Billing and Collections Series…
More Articles by Systems4PT
Busting PT Myths: “Physical Therapy is Just Exercise”
Busting PT Myths: "Physical Therapy is...
Busting PT Myths – Physical Therapy Is Only for Recovery
Busting PT Myths "Physical Therapy is...
Busting PT Myths – Physical Therapy Is Too Time Consuming
Busting PT Myths "Is Physical Therapy Too...