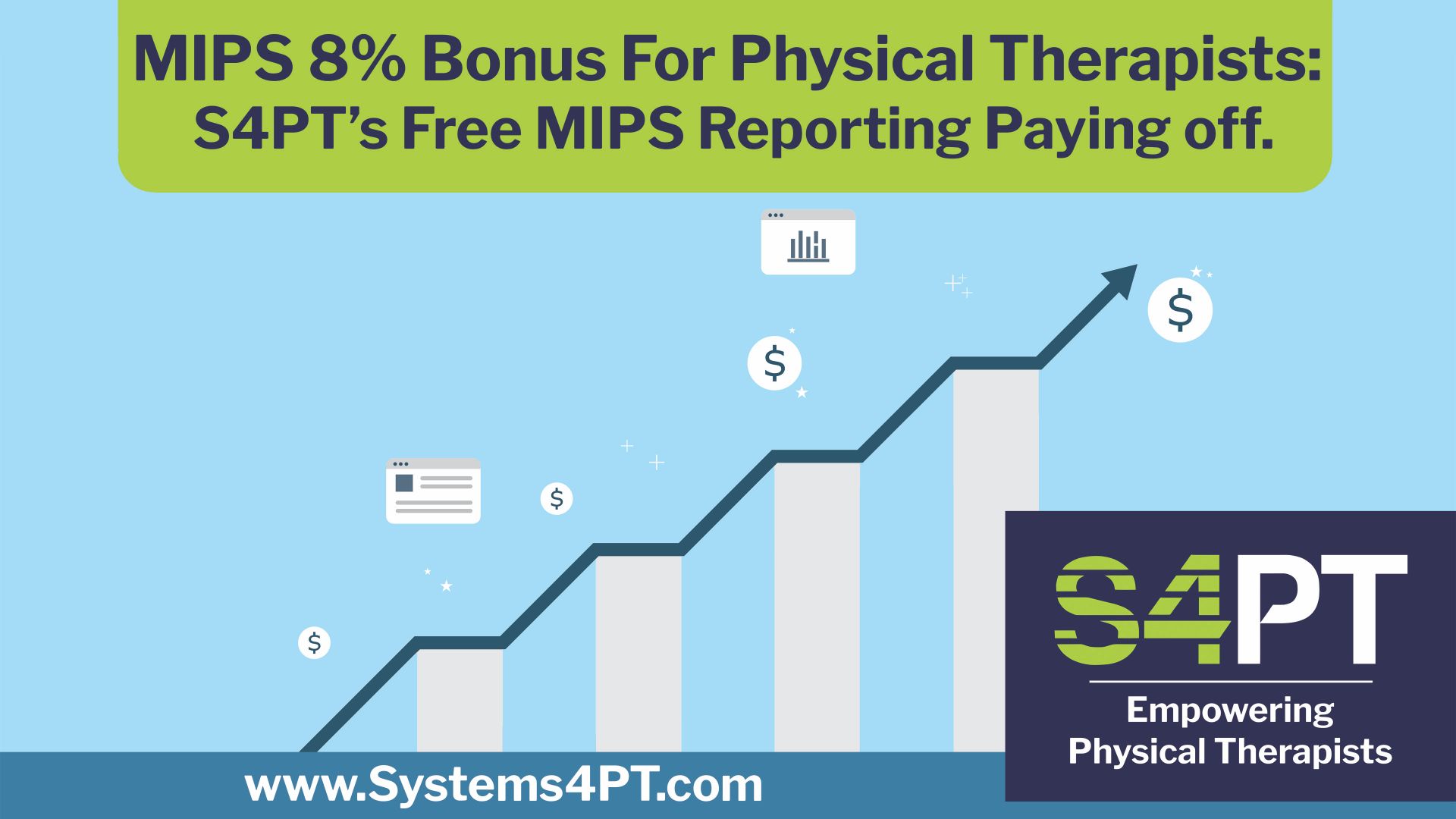
MIPS 8% Bonus Announced: Free MIPS Reporting for All S4PT Clients is Paying Off
In the world of physical therapy, opportunities to enhance your revenue should never be missed. At S4PT, we’ve been providing our clients with free MIPS reporting, leading to significant Medicare bonuses. This year, the maximum bonus has skyrocketed to 8.5%, and our clients are primed to cash in. But the benefits don’t stop there.
MIPS – A Critical Opportunity
The Merit-based Incentive Payment System (MIPS) rewards healthcare providers for delivering high-quality, cost-effective care. While the bonuses have been notable in the past, this year’s increase is a game-changer. Your MIPS participation in 2022 determined the bonus for 2024, highlighting the importance of immediate action and exceptional patient care..
Prepare for tomorrow Now
By actively participating in MIPS and prioritizing quality patient care today, you’re setting the stage for a rewarding future. Don’t miss this chance to make the most of Medicare’s increased bonuses.
What This Means for Your Practice
The additional bonus is not just a figure; it translates to real growth opportunities for your practice. Whether investing in state-of-the-art equipment or expanding patient services, the benefits are tangible..
S4PT – your Only Partner for Free MIPS Reporting
S4PT’s commitment to your success goes beyond words. Our free MIPS reporting is a testament to this commitment, helping you capitalize on this unprecedented bonus opportunity. We’re here to support you in delivering the best patient care, ensuring that our clients are well-prepared to reap the rewards in 2025.
Ready to take the next step? Reach out to us today and let us guide you in maximizing your Medicare rewards. Together, we’ll redefine what success looks like for your practice.
More Articles by Systems4PT
Real Cost of a Billing/EMR Solution for PT Practices
The Real Cost of a Billing/EMR Solution for...
Value Based Care is the future of healthcare reimbursement.
Value-Based Care is the Future of...
Billing vs Billing and Collections for Physical Therapy
Billing vs. Billing and Collections: Know...