Increased Reimbursements for Physical Therapy Clinics
An industry survey identified that the second greatest frustration for practice owners is declining reimbursements, which stem from a lack of control over payer authorization and billing clean claims. ” Better management” cannot fix this; the solution requires better technology. Increased reimbursements for physical therapy clinics are not a fantasy! Systems4PT has solved the problem!
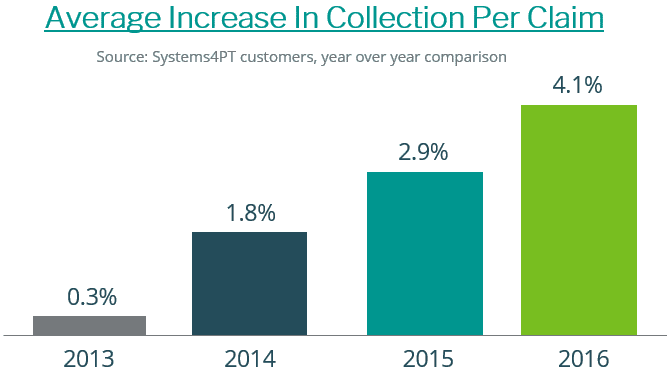
Most of the survey responses came from the EMR’s members/customers. While the survey respondents complained about declining reimbursements, Systems 4PT practices have seen average reimbursements per claim increase each year for the past four years in a row. We want you to experience the same increased reimbursements!
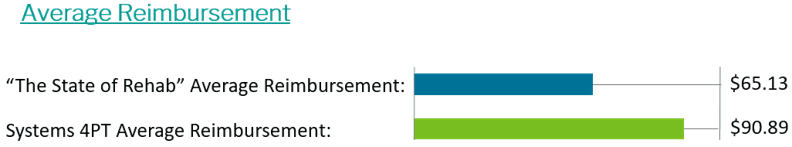
S4PT practices averaged $90.89 per claim nationwide in 2017
The Reasons You’re Experiencing Declining Reimbursements
1. Your EMR allows you to bill dirty claims
- Your low reimbursements prove that your EMR’s claim scrubbing is inadequate. It lacks the necessary payer rules.
- Required data is missing, ex. An authorization number.
- Other data conflicts with what the payer is expecting, ex. The patient’s name is entered as “Bob,” but the payer is expecting “Robert.”
2. Your EMR isn’t integrated with your billing system
- Deductibles and coinsurance due, do not transfer to the front desk. This costs you 5% of revenue (the front desk can’t collect them).
- CPT codes often fail to transfer from the EMR system to the separate billing system. If these codes are not submitted, you are not paid.
- The EMR calls this “HL-7 transmission errors”. We call this “Billing that isn’t integrated”.
- There are no scans or PHI in the non-integrated billing system – The biller is blind.
3. As a result, your biller spends most of their time on defense, finding, correcting, and rebilling rejection
- There aren’t enough hours in the day to get the work done.
- While your biller is busy reacting to dirty claims, payers continue to change their rules and requirements, ensuring future rejections.
- Payers are aggressively investing in technology; your biller is simply out-gunned.
How Systems4PT has Increased Reimbursements – Show your biller!
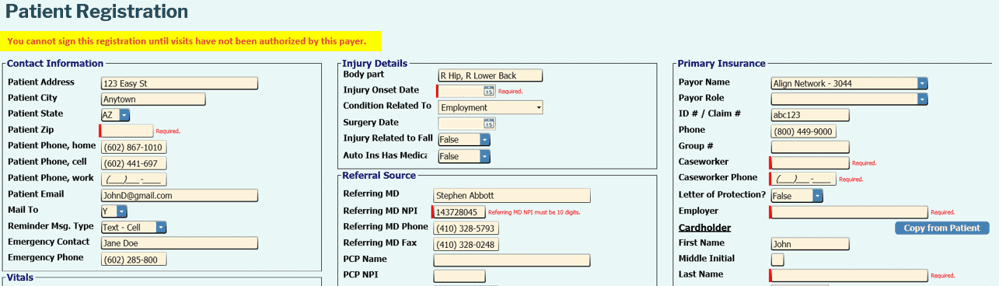
Systems 4PT delivers the most robust, real-time claim scrubbing in outpatient rehab. Both therapists and front desk staff are guided toward creating clean claims that satisfy payer rules.
As payers change their rules, we update the software. The registration below can’t be signed until all requirements have been satisfied
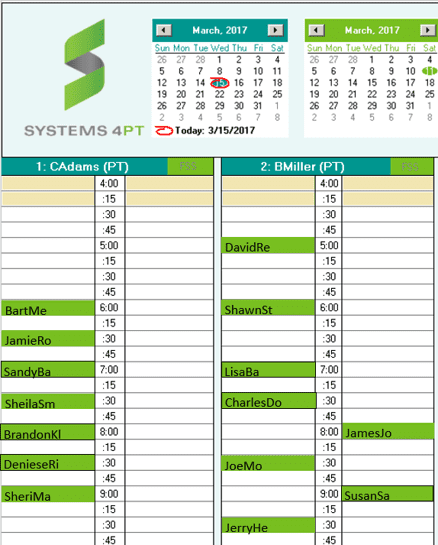
Green Patients Get Paid
When every payer rule has been satisfied, the patient turns green on the schedule screen. With Systems 4PT, the front desk’s job is to “Turn every patient green”. And when that happens, you’re paid for every visit
The Conclusion
- Slow documentation and declining reimbursements are critical problems
- Your EMR has fallen behind and is now holding your practice back
- Your EMR has become a liability
Systems 4PT has solved these problems, and we’d love to show you with our free, no-pressure demo. Your collections will increase by 9%, and you’ll pay 1/3 less than your outdated EMR and billing cost today. Fill out the form below, and one of our reps will contact you.

